Intravascular imaging catheters have become integral to the detection of abnormal or vulnerable plaque, a major problem in coronary artery diseases. Courtesy of Siemens Healthcare.
A team of researchers from the Erasmus University Medical Center in Rotterdam, Netherlands optimized the use of intravascular imaging in the detection of coronary artery diseases via catheters. They presented their work at the Diagnostic and Therapeutic Applications of Light in Cardiology 2018 conference held in San Francisco earlier this year. This presentation detailed how the team modified a catheter design for better light delivery and for the prevention of optical damage by combining two intravascular imaging techniques.
Why is such research necessary?
Cardiovascular diseases are on the rise. Specifically, coronary artery diseases (CAD) are a major medical problem, as well as the main cause of deaths worldwide. A major symptom of such diseases is the buildup of plaque on the walls of the arteries, narrowing the diameter of these blood vessels. As the artery narrows, it is increasingly difficult to carry blood or oxygen to the heart muscle.
Intravascular imaging catheters are necessary to identify vulnerable plaque in the arteries. Current imaging techniques such as intravascular ultrasound, intravascular optical coherence tomography and near infrared spectroscopy have proven unsuccessful in accurately identifying vulnerable and asymptomatic plaque. Therefore, researchers are now testing the success of combined intravascular photoacoustic and ultrasound (IVPA/US) imaging.
How does this intravascular imaging technique work?
Combined intravascular photoacoustic and ultrasound imaging uses both light and sound to identify the plaque. Intravascular photoacoustic imaging uses optical absorption contrast. It converts overtone vibrational absorption into thermoelastic waves. An ultrasonic transducer then detects these waves. By combining this technique with ultrasound imaging, researchers detect different components of abnormal plaque and create images on the structure of the interior arterial wall.
What components and specifications must the catheter meet?
Because transmitting light and receiving ultrasound are essential to the function of intravascular photoacoustic and ultrasound imaging, the catheter must contain a light delivery port as well as an acoustic transducer. Additionally, in order to have functional clinical use, the catheter must be small and flexible. It must be able to withstand the arterial environment. These specifications must be kept in mind during the design of the intravascular imaging catheter, particularly when considering materials.
How did the team from Erasmus modify existing designs?
The Erasmus team made two major modifications to the intravascular photoacoustic and ultrasound imaging . First, they improved the light delivery component. The light delivery method of choice is optical fiber. In previous designs, this fiber was 100 μm, but the newest design replaced it with a 200 μm fiber. A new optical rotary joint was designed in house to couple a stationary light beam to the rotating 200 μm fiber through a 50 μm air gap. This reduced optical and mechanical damage to the catheter and rotary joint surfaces observed in previous designs.
Additionally, the inclusion of a quartz tube to seal the fiber and prism, which deflected the light beam from the 200 μm multi-mode fiber prevented further optical damage. These modifications allowed the team to decrease the amount of laser light lost in the path. In previous designs, 60% of laser light was lost. In current designs, only 20% of light is lost.
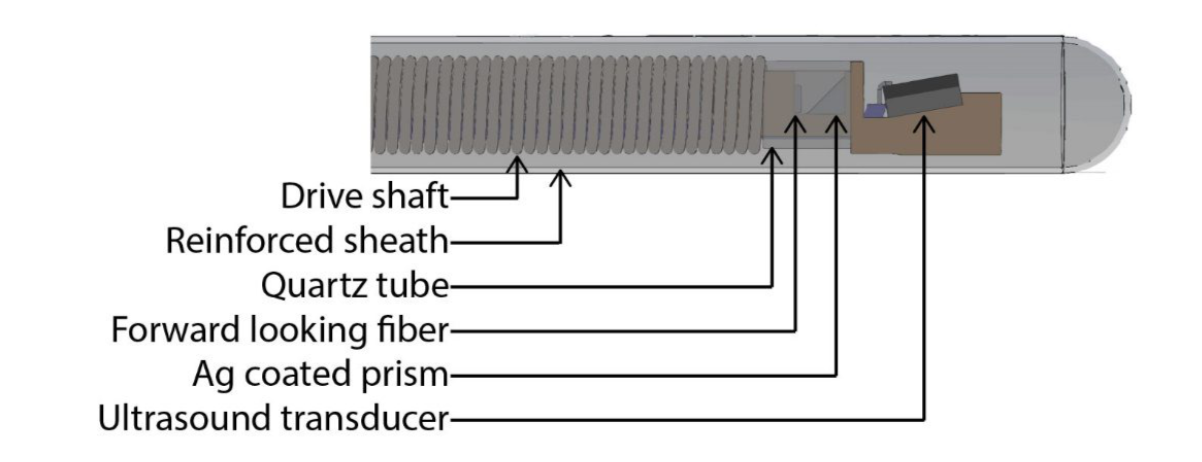
The above diagram details the components of the intravascular imaging catheter tip. Courtesy of SPIE Digital Library.
The team also modified the outer sheath of the catheter. The choice of material is important as it could cause further damage to the arterial wall. However, it must allow for ultrasound and light waves to pass through without disturbance and must provide enough support for interior mechanisms of the catheter. Polyethylene, fluorinated ethylene propylene, ethylene tetrafluoroethylene, and polytetrafluoroethylene were all tested as viable material options. Tests performed in water at room temperature at the wavelength of 1718 nm determined the one-way acoustic attenuation and optical attenuation. The most viable option based on these tests was the polyethylene sheath.
The Results
The newly designed intravascular photoacoustic and ultrasound catheter was tested on a human coronary artery sample. The images using the catheter were taken under various conditions: without polyethylene (PE) sheath in D2O saline, with PE sheath in D2O saline, without PE sheath in normal saline and with PE sheath in normal saline. The artery sample was sliced into 10 μm thick sections and then stained with Oil Red O to detect lipids. The filtered data from the catheter was compared to the stained coronary artery sample.
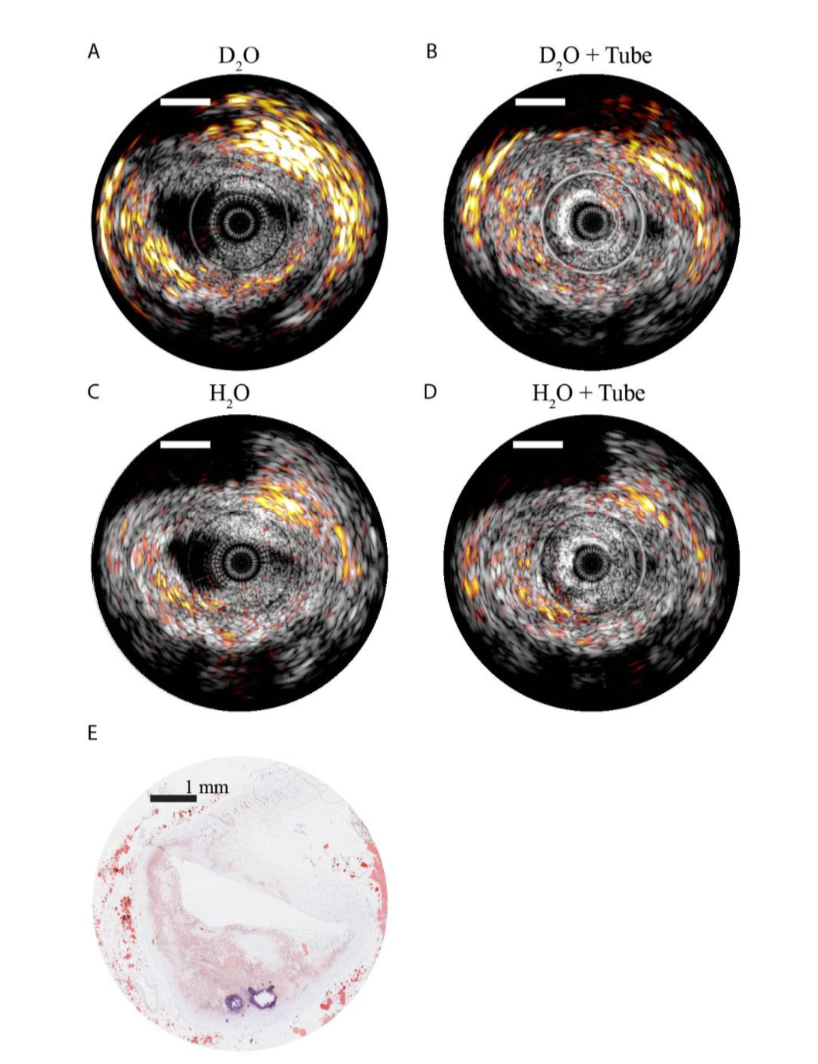
The images above show the processed data obtained from the catheter. Figure E is the histology after researchers stained the sample. Courtesy of SPIE Digital Library.
In conclusion, the sheath still has a negative effect on the photoacoustic signal. However, the research and studies were still highly effective in imaging lipid-rich plaque. The Erasmus group was also successful in creating a more robust catheter with more efficient light delivery. With improved sheath material and other small modifications, a intravascular photoacoustic and ultrasound catheter could soon have clinical applications.
For more information on this new medical technology, read the paper science paper.
