Two-photon excitation micoscopy (a.k.a. TPEF/ 2PEF) is the most common type of multiphoton fluorescence microscopy. It is a very interesting and useful technique for its ability to lock down on very specific and small areas. As well as that, it produces very high speed and high resolution results. This is ideal for biomedical applications that monitor very small structures. Hence, usages of TPEF range from tissue engineering to neurobiology. In this article we will discuss the principles and history behind two-photon microscopy and its biomedical diagnostic applications.
History & Principles
Two-photon microscopy was first discovered and patented at Cornell University in 1990. There, researchers by the names of Denk and Strickler were working with laser scanners in order to find a new way of imaging. The concept of two-photon absorption had been around for decades, but was only recently used as a tool in spectroscopy. Denk and Strickler pioneered two-photon microscopy utilizing infrared lasers and microscope objectives. Today, Ti-Sapphire lasers and Yb-doped fiber lasers are among the most popular choices for TPEF. This is a consequence of their high photon density and the principle behind TPEF.
The principle of two-photon microscopy can be described most simply as the simultaneous absorption of two photons by a fluorophore. It should be noted that this is a very rare event compared to single photon absorption. Thus, the incident laser’s photon density should be very high. In general, a high photon density will increase the probability of an event occurring. Consequently, only a high density will allow this rare event to occur a significant amount of times. Furthermore, the rarity of two-photon absorption plays key in the highly focused nature of TPEF. In other words, only the plane of focus in the material ends up with a significant result. Out of bounds areas do not have enough photon density to interfere with the results. Hence, two-photon microscopy produces a much clearer and accurate picture compared to its single photon counterparts.
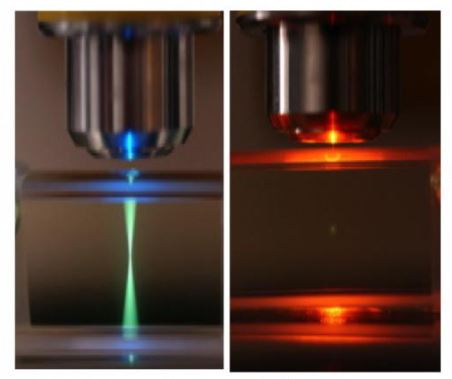
Figure on left: Singe photon confocal microscope exhibiting fluorescence from out of focus planes.
Figure on right: 2 photon microscopy exhibiting fluorescence from focal spot only.
Courtesy of Ruzin.
Two-Photon Microscopy Applications:
Diagnosing Skin Cancer
Skin cancer is an ever present and growing concern in the medical field. Existing skin cancer diagnostic methods require invasive (flesh cutting involved) and time consuming exams. As optical technology advances, more cost-effective and reliable diagnostic tools evolve. Some optical methods in usage include dermoscopy and fluorescence diagnoses. However, these techniques are limited to thin, outer layers of skin. This is due to the absorption and scattering of light by skin tissues. However, near infrared lasers can solve this issue because skin is not as affected in this spectrum. Among the microscopy techniques that utilize infrared light, is two-photon microscopy.
Two-photon microscopy applications have allowed cell morphology to be analyzed at depths and clarity not seen before its time. It is also noninvasive and has very little side effects on the patient’s daily life. TPEF has been utilized in several studies on patients with possible basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma. The studies showed that TPEF is able to image with as much depth as traditional histopathologic methods. Additionally, these study results showed positive patients had varied fluorescent activity in skin structures.
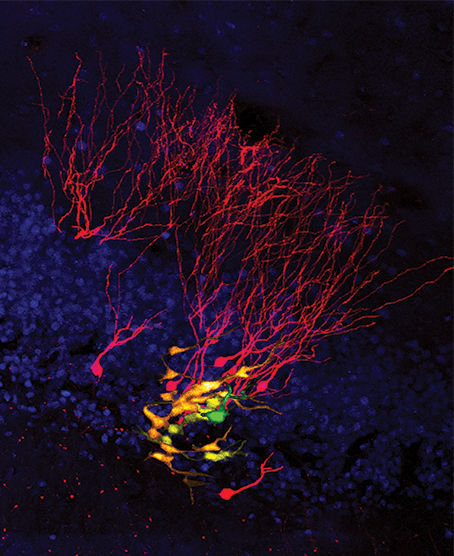
Image of an individual neural stem cell taken using two-photon microscopes. Generated daughter neurons are shown as yellow, orange, or red, depending on their age.
Courtesy of Science magazine.
In order for these study results to make much sense to us, we will discuss an aside. In healthy patients, the skin cells exhibit autofluorescence. Specifically, the cytoplasm material in the cells exhibit autofluorescence. This fluorescence intensity increases with skin depth. Thus, the uppermost layers, which are the stratum corneum (SC) and stratum granulosum (SG), are the least fluorescent. Further, we introduce the less bright lower layers: stratum spinosum (SS), and stratum basale (SB).
Diagnostic Results
In a study done by Paoli et al, SCC patients showed a abnormally thick stratum corneum, with fluorescent nuclei and areas of bunched up keratin. Next, these patients also exhibited irregularity in lower skin layers (SG, SS, SB). Specifically, the keratin cells inside these structures were abnormally far apart. As well as that, they showed multiple nuclei within each cell. Further, abnormal keratin cells were observed to fluoresce much brighter than surrounding cells. Many lesions in this study also contained a strange, speckled fluorescence within cells in lower layers. Undoubtedly, there were some issues in the study as most studies have. Namely, patients with BCC were included in testing. However, imaging was difficult due to the large amount of thickened keratin structures. Along with BCCs, nodular BCCs (nBCC) were also not able to be studied in detail. This is because much of the lesions were out of reach their lasers.
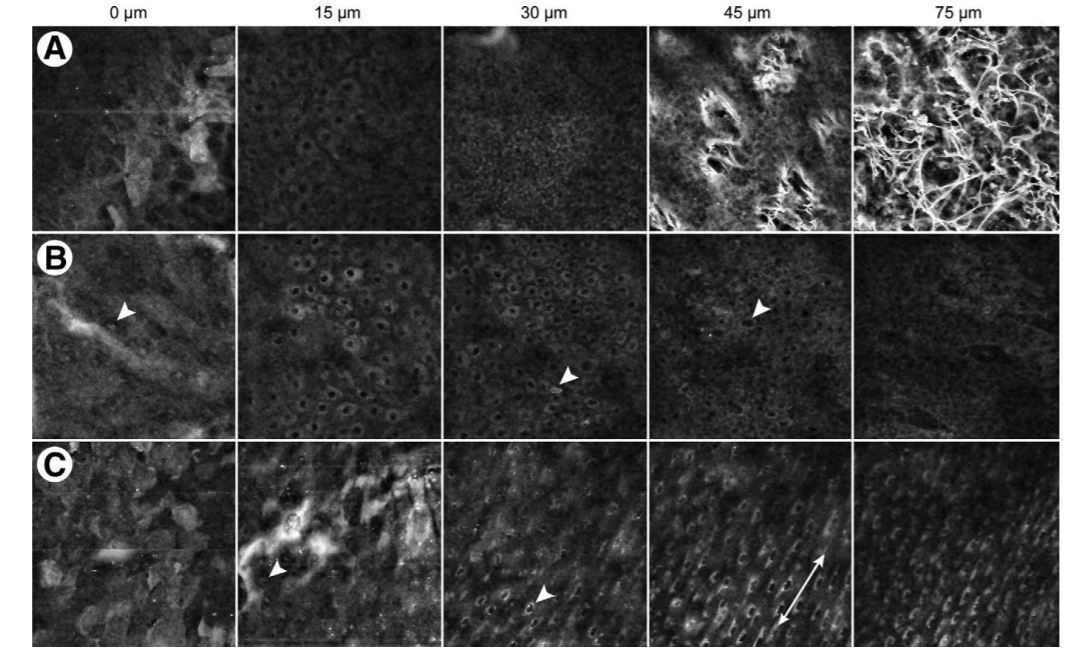
TPEF images of (A) normal skin, (B) SCC in situ specimen, and (C) SBCC specimen.
Courtesy of Journal of Investigative Dermatology.
Conclusion
Two-photon microscopy is a technique that allows for focused, high resolution imaging. In the biomedical market this translates to quick and accurate medical diagnoses. On the other hand, in the dermatology market TPEF can eradicate invasive and resource consuming diagnostic procedures. Future possible skin cancer cases could be diagnosed with a quick scan. This would be much more convenient than a laborious tissue cut and exam process. There would be no patient downtime for tissue healing and waiting around for a diagnoses.
Current studies show that improvements do need to be made on TPEF instruments. For skin BCC diagnoses, a deeper laser penetration length would allow for more complete visualization of deep growing lesions. Higher energies may cause tissue damage, so the technique needs to be refined at safe laser levels. Another improvement that could be made is possibly reducing the size of the microscope (less than 2mm). This would also help capture difficult-to-reach and uneven skin tissues.
This post is sponsored by Connet Laser, the leading manufacturer of fiber lasers and amplifiers.
