Minimally invasive surgery is typically the most desirable option when getting a surgical procedure done. Mayo Clinic reports that a patient will typically experience less pain and encounter fewer complications when opting for a minimally invasive procedure. These days, minimally invasive procedures can be performed by doctors aided by robotic tools. One such tool is the da Vinci Surgical System.
Assumedly, the da Vinci name pays tribute to one of the greatest and most inventive minds known to history, Leonardo da Vinci. Da Vinci is a system developed by a company named Intuitive—a self-proclaimed pioneer in robotic-assisted surgery. And indeed, they are. Let us explore how minimally invasive procedures have evolved and progressed to the point of the da Vinci platform.
Da Vinci Systems
Intuitive launched the da Vinci system in 2000 and has since released four generations of system. The most recent generation offers three different models. The capabilities differ by model, as well as by the system’s versatility. However, each model is comprised of a patient cart, surgeon console, and a vision cart. The patient cart features the robotic arms that carefully wield the surgical tools controlled by the surgeon. The surgeon console allows the surgeon to oversee all of the tool motions and positions. It allows the surgeon to view, access, and control the instruments that are outfitted to the console for the respective surgery. The vision cart is the center of communication and power generation of the components of the da Vinci system. It can perform image processing and includes a screen to allow a live view of the surgery for others in the operating room.
One of Intuitive’s da Vinci systems. Courtesy of Drugwatch.
Early Cystoscopes
It is only because of centuries of development in minimally invasive procedures that the medical world could arrive at robotically assisted surgery today. Minimally invasive procedures arguably began with cystoscopy. The earliest cystoscopes were fashioned by Phillip Bozzini in 1806 who was a surgeon for the German army. His device was used to view the throat, and later, was used in urology. His rudimentary cystoscope involved strategically angled mirrors and used a candle to illuminate the inside of the body. He called his device the Lichtleiter. This quite literally translates to ‘light leader’ or ‘light guide’. From there, it took until 1878 for a more modern cystoscope to be developed. This was achieved by Maximillian Nitze and Josef Leiter. Inspired by a microscope eyepiece, they designed optics similar to a telescope that could be illuminated with a platinum wire filament.
From there, other scientists and doctors began to design better cystoscopy and endoscope-like devices. Georg Kelling of Germany used an endoscope to examine a patient’s abdomen in 1901. This was the beginning of laparoscopy. It is said that he performed such laparoscopic procedures as many as 45 times to diagnose patients. At the same time, Von Ott over in Russia used a cystoscope for gynecological purposes.
Endoscope Evolution
The 1920s ushered in a major contributor to the progression of laparoscopy, Heinz Kalk. He is colloquially dubbed the “Father of Modern Laparoscopy”. This was in reference to his design of, what was at the time, a “superior laparoscope with improved lenses”, as well as a method of safely taking liver biopsies. His design included foroblique optics which allowed for a 135-degree view. With such a wide viewing angle, rotation of the instrument allowed a surgeon the full view around the body cavity. Until then, most endoscope had viewing angles limited to around 80 to 85 degrees. Kalk’s design was so effective it was not dramatically improved upon over the next thirty years.
Despite Kelling’s success and Kalk’s wide view endoscope design, it took time before laparoscopic surgery techniques were widely and readily embraced. The primary usage of endoscopes was limited to gynecology even through the 1960s and 1970s. In the 60s, the endoscope underwent another redesign. Influenced by Harold Hopkins and Karl Storz, the endoscope became a combination of a rod-lens optical system with bundled fiber optics. This design effectively made the endoscopes cold light illuminated. Cold light illumination refers to sources that do not have an appreciable heating effect. Gone were the days of illuminating the instrument/body cavity using open flames or dangerously hot filaments. These newer endoscopes also transmitted a clearer and larger image than its predecessors.
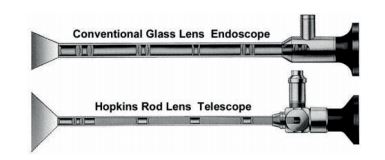
Side-by-side cross-section of a lens-based endoscope compared to Hopkins’ design. Courtesy of De Greon.
Another factor that influenced laparoscopy was the evolution of computer technology. In the 1980s, computer chips made it possible for images to be magnified and projected onto television screens. 1983 saw Welch Allyn produce the first endoscope using a CCD sensor. The sensor was positioned on the end of the endoscope. The body cavity could then be detected and imaged by the sensor, the detections turned into a digital signal, and then finally processed and displayed. Now, it was simple for many in the operating room to view what was happening in surgery. This later progressed into video capsule endoscopes. Some video endoscopes contain multiple CCD cameras that can create a full 360-degree image.
If you enjoy this article, you might also want to check out our post on the role of fiber optics in medicine.
Robotic Surgery, da Vinci and Before
Technology and computing continued to improve, and with that came the advent of robotic surgery. The first FDA approval of robotic surgery equipment occurred in 1994. The administration approved the Automated Endoscopic System for Optimal Positioning, or AESOP. AESOP assisted with endoscope positioning as verbally directed by the surgeon. From there, other robotic systems like da Vinci were created and later approved for use.
This brief history hopefully sparked a greater appreciation of the centuries of development in minimally invasive surgery that ultimately led to Intuitive producing da Vinci in 2000.
