
New research suggests that non-ablative fractional lasers (NAFLs) could give doctors a new tool for treating early-stage colorectal cancer. Picture courtesy of http://www.drreddyforlife.com/2016/08/24/use-tips-improve-doctors-office-visits/
A group of South Korean researchers recently published research revealing a new and innovative way to treat colorectal cancer and precancerous tissues using non-ablative fractional lasers (NAFLs). This new approach could allow physicians to treat and prevent early-stage colorectal cancer, while also reducing the risk to their patients, with the help of this minimally invasive technique.
According to the American Cancer Society, colorectal cancers are the third most common type of cancer and are the second deadliest. Though these statistics may seem grim, the outlook has been improving for those diagnosed. The mortality rate of colorectal cancer has declined by more than 50% over the course of the last few decades. This significant reduction in deaths is due in large part to regular colonoscopy screenings. These regular exams can allow doctors to detect cancerous cells before more prominent symptoms appear, increasing survival rates.
During these screening procedures, the entire length of the colon is examined for tumors and precancerous tissues, called polyps. If any are found, they are forcibly excised with the aid of a small, sterile wire snare and an electric cautery machine. This prevents the cancer from spreading to other parts of the body and developing into a more advanced, and deadly, stage.
While this procedure is generally very safe for patients, it is still not without its risks. Some possible complications of polyp removal during colonoscopies are relatively minor, such as easily-controlled bleeding, while some are as significant as a perforation, or tear, in the colon wall. Another concern for patients is that if polyps are not completely removed, they could grow back. In this case, additional medical interventions and more frequent colonoscopies are necessary. In contrast, NAFLs are not thought to pose these major risks and could be much safer.
Non-Ablative Fractional Lasers (NAFLs)

Non-ablative lasers allow for the specific targeting of cancerous tumors, while leaving nearby, heathy tissues intact, picture courtesy of https://www.laserlevelhub.net/green-vs-red-beams-laser-level-which-is-better/
Fractional lasers are a type of laser that are commonly used by dermatologists to treat patients with cosmetic skin complaints, e.g. scars or wrinkles. These lasers work by heating very small regions of body tissue to create Microscopic Thermal Zones (MTZs). Because these MTZs are only a couple hundred µm in diameter, nearby healthy cells are relatively unaffected. These lasers are divided into two major classes, ablative and non-ablative lasers. Ablative lasers produce lower energy light, but kill all layers of human skin cells. Because of this damage, it takes patients longer to recover from ablative laser treatments than from non-ablative lasers, which do not destroy skin cells. Rather than killing human tissues, the NAFLs affect skin cells by inducing the human body’s wound response and encouraging healing in the area targeted by the laser.
The Effect of NAFLs on Healthy Tissue
While the results of this study suggest that NAFLs could potentially be used to treat early-stage colon cancers and limit tumor growth, current research is uncertain about whether and to what extent NAFLs could affect healthy bowel tissues. This is especially true, given that these researchers were uncertain about which biological mechanisms the NAFL lasers were interrupting in the cells they targeted.
Because NAFLs are known to primarily affect biological tissues by heating them, these researchers also monitored the tissues in the experimental condition for heat-related changes in targeted and nearby tissues. They found that, while the temperature of tumor sites did indeed increase dramatically, the temperature increases that neighboring tissues experiences were significantly smaller, and that they returned to normal over the span of a few seconds. Given that thermal damage is the most likely threat to nearby healthy tissue, this experiment does not provide evidence to indicate that non-cancerous tissue would be negatively impacted by the use of NAFLs.
Study Design
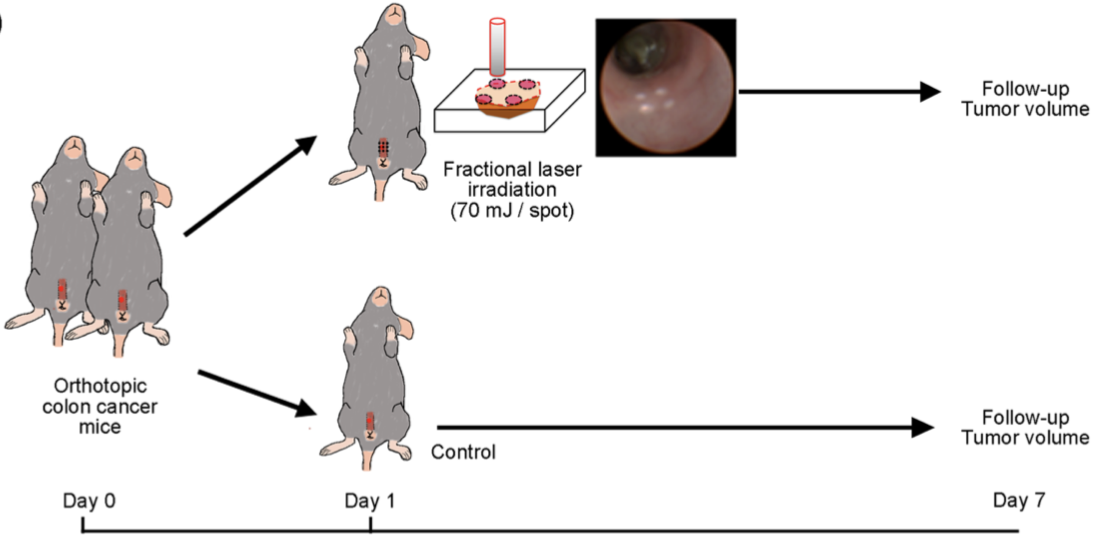
South Korean researchers’ study observed the effect of fractional laser irradiation on colon tumor growth, compared to a control group, over the span of a week. Picture from https://www.nature.com/articles/s41598-018-19792-2.pdf
In the South Korean study mentioned above, researchers evaluated the potential for non-ablative fraction lasers to treat early-stage colorectal cancer by testing the technique in early-stage colon cancers in mice. To ensure uniformity of disease, progression, and cancer location, all mice had the same type of cancerous cells (SL4-DsRed) endoscopically implanted into their colon. After allowing the cells time to grow and assimilate into the colon’s epidermis, mice were irradiated with NAFLs. Over the course of a week, the mice’s colons were monitored for tumor growth with both white light and fluorescence imaging.
Results
The difference in tumor growth between the experimental and control group was visually assessed. On each day for a week, tumors were assigned a numerical score corresponding to the tumor grade. When these ratings were compared by researchers, they found 6 and 7 days after the transplantation of tumor cells, the group of mice irradiated with NAFLs had tumors that were growing significantly more slowly than the control group that had not been irradiated.
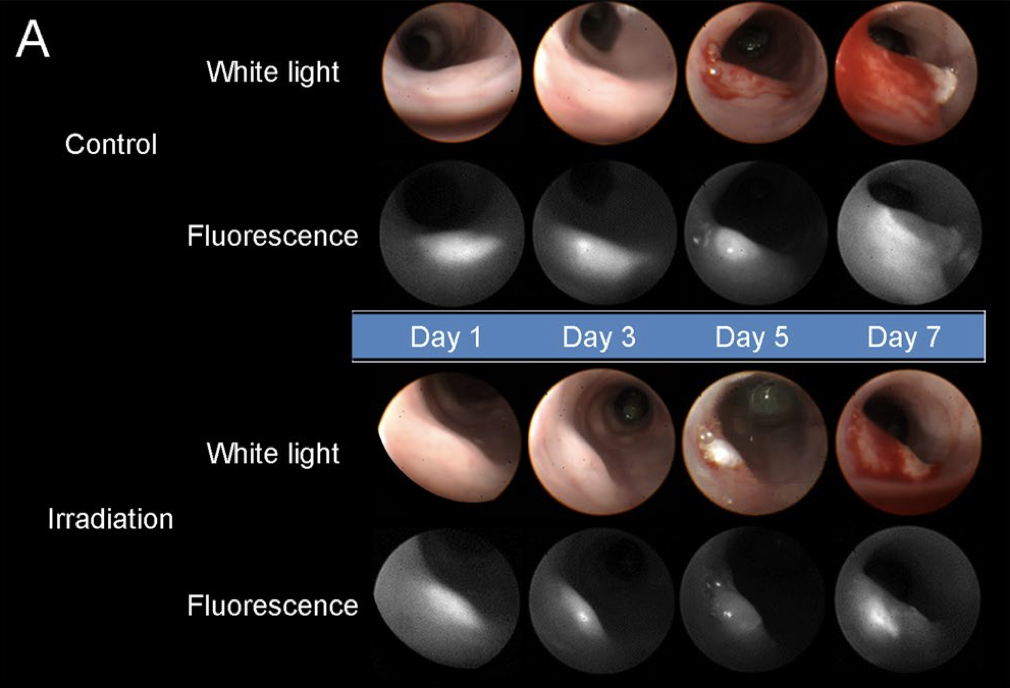
The results of this South Korean study show a clear reduction in the rate of tumor growth in the mice exposed to irradiation by NAFLs. Picture courtesy of https://www.nature.com/articles/s41598-018-19792-2.pdf
The figure above illustrates the difference in the progression of tumor growth within the colons of mice. In the early days following transplantation, tumor growth appears to be relatively similar. By the fifth day, though, the size of the tumor appears much larger in the mice that were not irradiated. Given the difference between the two groups, the researchers concluded that further research should be done to investigate the potential for NAFLs to be used to treat similar early-stage colorectal cancer and to determine the optimum therapeutic dose of NAFL. Still, this research seemed very promising and showed one more way that NAFLs have the potential to be used in modern medicine.
To read more about this study & the research team’s use of non-ablative fractional lasers to treat early-stage colon cancer, click here.
