If you’ve visited an optometrist, they may have used optical coherence tomography (OCT) to scan your retina. This new technique uses low coherence interferometry to image semi transparent tissue. Being a noninvasive technique has the added benefits of being able to image tissue that is otherwise dangerous or impossible to sample with a biopsy. This makes OCT a powerful tool for diagnosing disease. In this blog post, we will introduce OCT and the various ways it’s currently being used in the medical field, as well as some benefits and limitations:
- How does Optical coherence tomography work?
- How is OCT used in optometry?
- How else can OCT be used?
- Benefits and Limitations of OCT
How does Optical Coherence Tomography work?
Optical Coherence Tomography is often compared to ultrasound, as they both use waves to image organs and tissue. However, the key difference between the two is that ultrasound uses sound waves, which move by compression and rarefaction of a medium. During an ultrasound procedure, a transducer converts electrical signals into ultrasound waves that are aimed at the target tissue. These waves travel much slower than light and the echo created by the sound wave, as it bounces off the target tissue, can be measured accurately. In contrast, OCT uses light waves which travel on the order of 10^8 m/s, making it impossible to detect time delays for light traveling a few millimeters. OCT uses interferometry to measure the time delay of the traveling wave, which has the added benefit of greatly increasing the resolution of the image.
OCT uses a type of interferometry called Michelson Interferometry, seen in the image below. In the simplest version of this interferometer, a beam of light is split into a reference beam and a sample beam and sent towards two mirrors. The reference beam is directed at a fixed mirror and reflected back towards a detector. The sample beam, on the other hand, is reflected off a movable mirror, which can be adjusted along the path of the beam. Since any change in the path length of the light beam is directly related to the change in the phase of the beam, the two beams will interfere with each other. This allows for measuring small changes in distance.
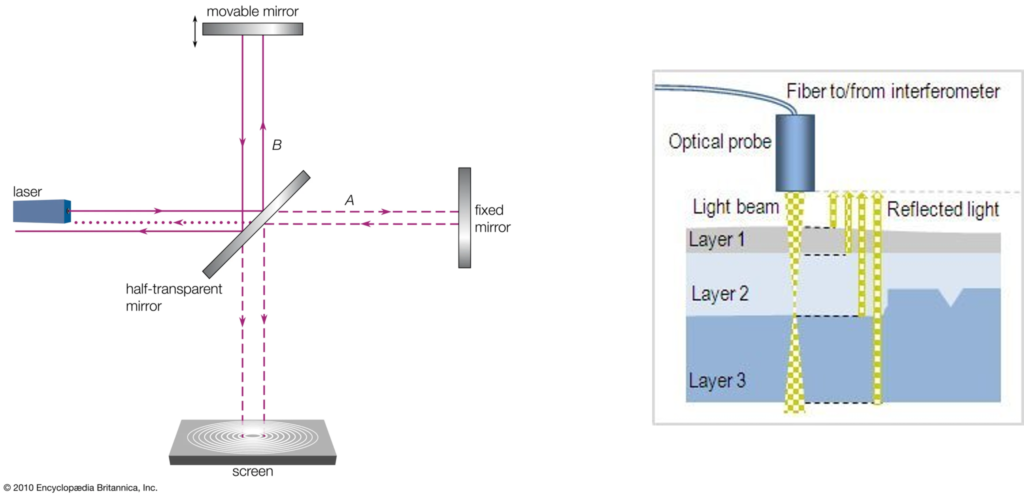
(LEFT) An illustration of a Michelson Interferometer. Courtesy of Britannica. (RIGHT) An illustration of low coherence light incident on a multilayer, semitransparent sample. Courtesy of Novacam.
In the case of OCT, rather than using a mirror to reflect the sample beam, the target tissue scatters or reflects the light back to the detector. In most cases, the incident light is a gaussian beam with a large bandwidth spanning several wavelengths of light (visible or near-infrared). Light with a large bandwidth will have low coherence. When low coherence light is incident on a sample of multiple semi-transparent layers, such as in tissue, the different wavelengths of light reflect at difference boundaries, as can be seen in the image above (right). It’s important to note that there are two types of images that result from an OCT scan. An A-scan is the cross-section produced when scanning the tissue. A B-scan is obtained by compiling a sequence of A-scans across a region into a larger image that shows the structure of the tissue from above.
There are three types of OCT that can be used during an examination: time domain, spectral domain, and swept source OCT. Time domain OCT uses fewer images than spectral domain OCT, which are spaced apart (this is illustrated by the green lines in the above image). Spectral domain OCT continuously captures images of the region of interest, and is related to time domain OCT through a Fourier transform, which can be performed using a FFT function on a computer. Swept source OCT, as it sounds, sweeps through a range of frequencies and records the tomographic information. Today, most OCT machines use a combination of spectral domain and swept source OCT.
How is OCT used in optometry?
Currently, optical coherence tomography is mostly used in optometry for retinal imaging to screen for various eye diseases, like glaucoma or diabetic retinopathy. During an exam, pupil dilation is important to allow as much light to enter the eye as possible. Then, an optometrist scans the retina in a series of cross sections. These cross sections are then compiled into a surface view image (B-scan). This details the various layers of the retina, and can reveal disease, which is especially important since the retina cannot be biopsied.
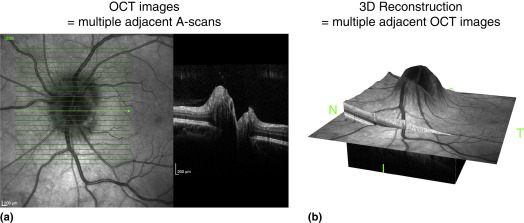
(a) An example OCT B-scan (left) of a retina compiled from multiple A-scans (right). (b) A 3D reconstruction of the OCT scan in (a). Courtesy of the Encyclopedia of the Neurological Sciences
There are several current uses of OCT for detecting disease, the most common of which is glaucoma. Glaucoma results from excess fluid present in the eye, creating an imbalance in the eye’s internal pressure. When using OCT to look for symptoms of glaucoma in a patient, an optometrist looks for signs of pressure buildup. This looks like a widening of the optic nerve or thinner tissue layers.
OCT is also used when looking for diabetic retinopathy, caused by damage to the blood vessels in the retina. It’s also used for detecting macular puckering, holes, and degeneration due to aging. These are structural issues in the retina that cause loss of vision, and can be seen easily through OCT.
Other uses of OCT?
As a noninvasive technique there is a lot of desire to find other uses for OCT in medical imaging. Here, we will discuss uses for examining blood vessels (OCTA) and nontransparent tissue:
Optical Coherence Tomography Angiography (OCTA)
Angiography is the examination of blood or lymph vessels. When OCT is applied to the blood vessels in the retina, the light is reflected off moving blood cells. Traditional angiography, fluorescein and indocyanine-green angiography, is invasive as it requires injecting dye into the target region. OCT on the other hand is noninvasive, and requires less time to acquire an image since dye takes time to properly cover the region of interest.
Unlike a typical OCT scan, OCTA requires several scans of the same region to visualize the blood flow in the vessels. This introduces a complication where patient movement and blinking can create artifacts in the image. This can be fixed by using high sample rates (taking images over a very short period of time) or by using a spectral domain OCT.
Often OCTA performs like an improved OCT scan, though there are some unique benefits associated with the technique. For example, in 2019, Duke Health released a study that shows OCTA can be used for detecting Alzheimer’s disease in patients, who have a lower density of blood vessels in the retina than healthy patients.
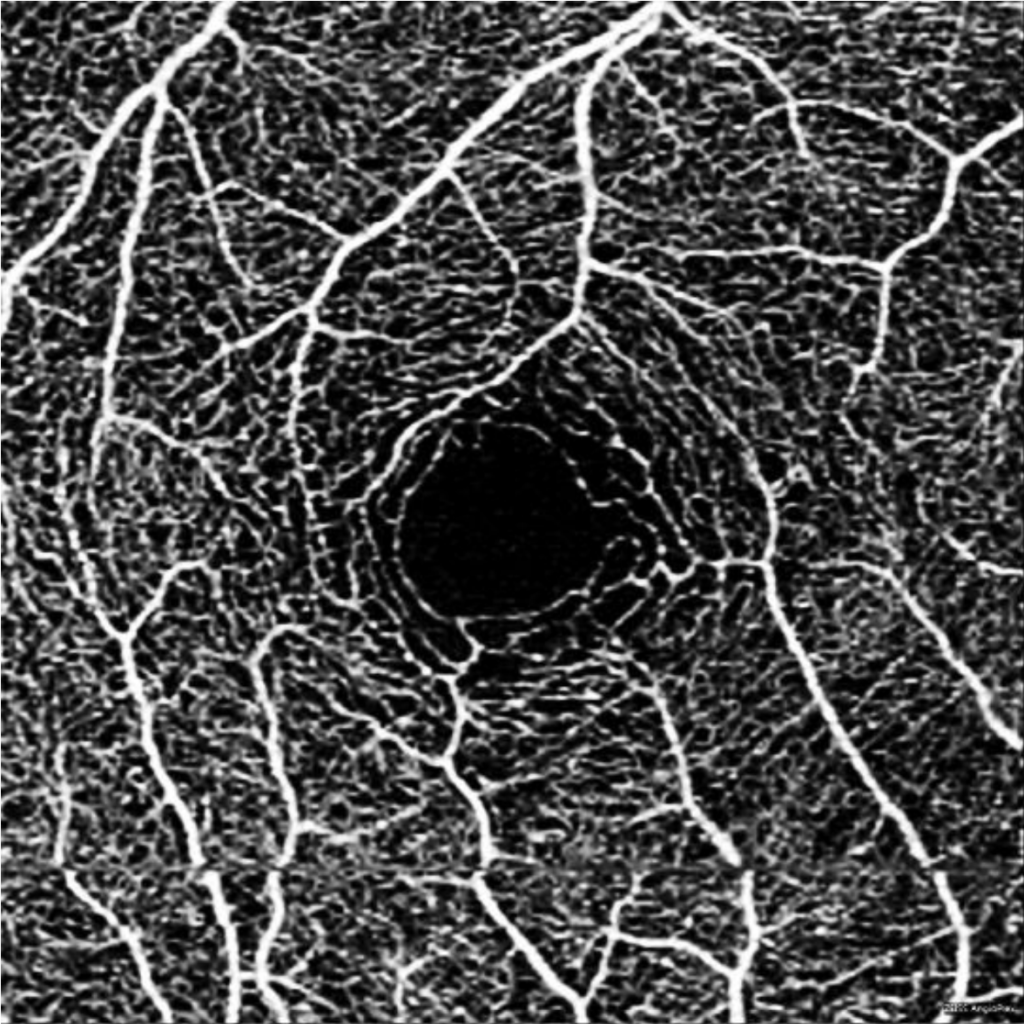
An OCT Angiogram of a health eye, detailing the vascular structure of the retina. A discontinuity artifact can be seen near the bottom of the image. Courtesy of the American Academy of Ophthalmology
OCT for non-transparent tissue
There has been a lot of research into using OCT with non-transparent tissue, with hopes that it can be used for preliminary screening of cancerous tissue or for imaging tissue that cannot be biopsied. Since there is no need to extract a sample from the subject, areas that are dangerous or impossible to biopsy will have accurate imaging. Though non transparent tissue absorbs most visible wavelengths, there are wavelengths in which it is transparent. Specifically at longer wavelengths of light (e.g. near-infrared), less light scatters off the scanned tissue. Instead, light penetrates the tissue before being reflected. The optimal wavelength of light depends on the properties of the tissue, but near 1300 nm works well in most cases.
Benefits and limitations of OCT
It is unlikely that OCT will replace traditional biopsy. However, it provides a useful tool for examining tissues for diseases, especially those that are dangerous to biopsy, such as brain tissue. It also helps in situations where other forms of imaging or diagnosis give high rates of false-negatives. The high resolution images from OCT provide more detail that can be missed in lower resolution imaging. Lastly, since OCT produces images in real time, it can be used during surgical procedures to provide additional information and guidance.
Since OCT requires light propagation, it is not useful in cases where light would be obstructed, such as by cataracts. These situations require a different technique. OCT is also limited in the axial resolution, or the longitudinal resolution. Light can only penetrate tissue up to a few millimeters, which is usually comparable to biopsy depth. However, this becomes an issue when the target region requires imaging a larger depth. Finally, patient movement also limits the effectiveness of OCT, since it can create artifacts in the final image. Many OCT machines have calibration software that minimizes the effects of patient movement, but some cannot be mitigated. For instance, if a patient blinks during the scanning there will be a black line in the B-scan. The only way to fix this is to scan the missed area again.
This post was brought to you by Connet Laser Technology - a leading manufacturer of fiber lasers
