Lasers came into the field of ophthalmology in 1961, when Ruby laser was used to create ocular lesions in rabbits. Unfortunately, creating vascular lesions in the human retina was not effective at that time, as blood poorly absorbs Ruby’s 694 nm red light. This was remedied with the discovery of Argon laser to give laser emission in the blue and green parts of the spectrum. Increasing the energy at these wavelengths can cause photocoagulation which can be used to treat retinal bleeding.
Diabetic retinopathy is a retinal disease in which blood vessels bleed into the eye. Photocoagulation is the common process induced by lasers to stop this bleeding. In this case, it is used to seal away the bleeding vessels.
In this article we will discuss how lasers bring about photocoagulation; the nature of diabetic retinopathy and how photocoagulation helps. We will also look into the common lasers used to treat such diseases in ophthalmology.
Photocoagulation
Increasing the energy of the laser beam so that tissue is heated to temperatures above 50 C, but below 100 C causes the proteins to denature and thrombocytes to initiate coagulation. This processing is called photocoagulation. It turns out lasers can be used to achieve this, but care must be taken to maintain the temperature so that vaporization does not take place, and the spread of energy is minimized to the surrounding areas. The image below shows the zones around the region of application as the laser beam energy is increased.
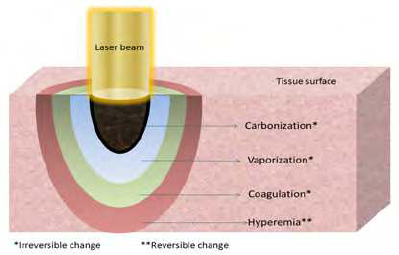
Zones of decreasing thermal effects. Courtesy ResearchGate.
Diabetic Retinopathy
Diabetic retinopathy is characterized by the rapid formation of new, poor quality blood vessels. This is called neovascularization. The new vessels grow into the surrounding portion of the eye and may obstruct the visual path. Also, the poorly formed vessels can leak blood into the surrounding regions. These blood vessels in the retinal circulatory system are sensitive to changes in the oxygen supply. The retinal vessels adjust their flow to maintain the tissue oxygen level. Diabetic retinopathy can be remedied if the oxygen supply is increased causing the retinal vessels to decrease their flow and stop the hemorrhage.

Diabetic retinopathy with a proliferation of retinal vessels. Courtesy Wiki.
Treatment works by using lasers tuned to the blood’s absorption wavelengths. Since blood absorbs blue and green wavelengths, argon laser at 488 nm and 514 nm can be used for treatment. The result of the laser interaction is coagulation that seals the blood vessels and stops the bleeding. The “destruction” of rods and cones on the retina during photocoagulation allows more oxygen to reach the inner retina, thus facilitating coagulation and constriction of the retinal vessels. Moreover, the increase of the oxygen supply in the eye fosters the constriction of the blood vessels further suppressing neovascularization. This gives us hope that a long term cure can become a possibility, instead of a short term treatment to just stop the bleeding.
Characteristics of Light in the Human Eye
For a successful treatment, the laser light must first reach the retina. To pass this hurdle, the laser beam must pass through the cornea, lens, and liquid in the eye ball to reach the retina in the back of the eye. This creates a unique requirement on the permissible wavelength range for the lasers that could be employed for this purpose. As the image below shows, only wavelengths close to the visible light interval till about 830 nm are transmitted to the retina.
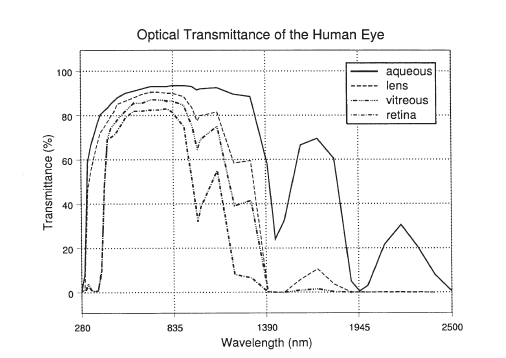
Transmittance of various wavelengths across the cornea, lens, vitreous humor till the retina.
Schematic Description of Photocoagulation
A typical setup involves a laser beam passing through a delivery system and creating an array of coagulated dots around the main central optic region. Above all, care is taken to avoid the the fovea and the optical disk that maintain the essential optical functions while the surrounding cones and rods are destroyed during photocoagulation. The setup below illustrates how the laser light is directed to the bleeding spots in the retina to achieve coagulation.
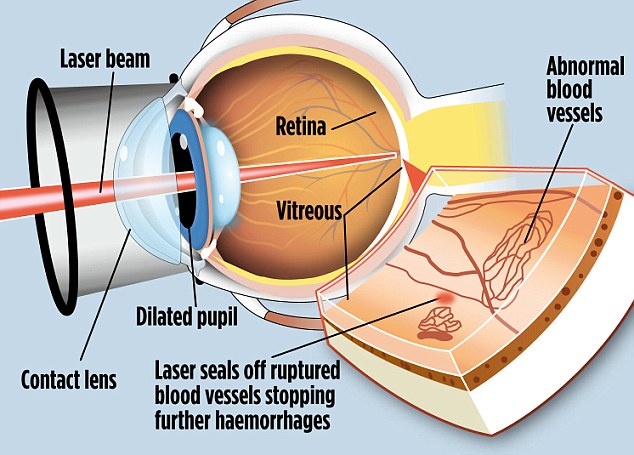
Setup for the laser delivery to photocoagulate spots at the ruptured retinal vessels. Courtesy DailyMail.
The result of a photocoagulation process using Argon laser is shown in the image below.
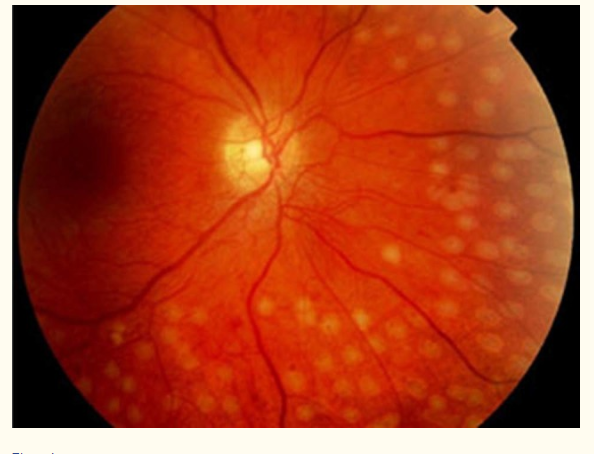
An array of coagulated spots formed around the main optical region. Courtesy AAO.
The fundus image of the eye shows the array of coagulated dots around the main central optical region. Neovascularization is suppressed as no extensive proliferation of retinal vessels in the eye is observed.
Typical Lasers Used in Photocoagulation
Laser light for photocoagulation must satisfy two criteria: reach the retina, be strongly absorbed by blood. Based on the light characteristics in the human eye, wavelengths around 300 nm to 830 nm can reach the retina. However, since blood reflects red light, it is not strongly absorbed around 630 nm. Using Argon laser with a lower wavelength around 480 nm, or diode lasers at a higher wavelength around 800 nm is a better choice. These wavelengths satisfy both criteria: reaching the retina, and being strongly absorbed by blood.
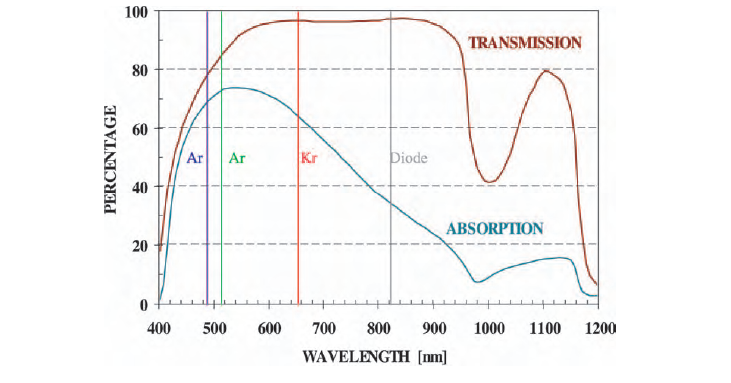
Different laser choices and their wavelength characteristics in the eye. Courtesy GlobalPedioLaser.
Since wavelengths other than red and not too far in the infrared work, Halogen lasers such as Argon are a typical choice for this purpose. However, the recent advancement in diode laser technologies make them competing candidates as they are very controllable and capable of delivering moderate energies for heating tissues. Diode Lasers have the added advantage of being less expensive, more compact and energy efficient in usage.
Check out FindLight’s collection of diode lasers and gas lasers for applications related to laser tissue heating, and ophthalmology. If you liked this article you might also be interested in our Comprehensive Guide on Gas Lasers.

hi
this is nice article and good knowledge
PATHOLOGY