Tissue welding is a relatively new procedure that aims to seal wounds and openings in a surgery using laser. The first tissue welding application using lasers was done in 1964 to join small blood vessels together using Nd:YAG laser. Since then many improvements have been put forward based on different medical fields.
Stitches and sutures are still the common ways to close wounds and openings in surgeries. They face the risk of contamination and reopening of tissues if the stitches are not held tight. Tissue welding using lasers removes all these complications by leaving minimal scars, leaving no entry for infections to permeate. Moreover the regions heal faster after surgery.
In this article we will discuss the mechanism behind tissue welding and the common biological solders and lasers used for this purpose.
Coagulation
Coagulation is the heating of tissues above 50 C and below 100 C to bring about denaturing of biological compounds. For example, proteins can break away from their quaternary structure and become long tangled fibrous substances. The image below shows collagen becoming denatured with temperature.
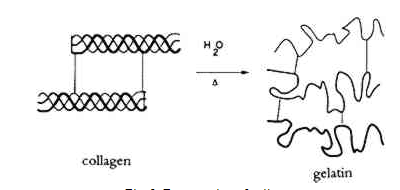
Denaturation of proteins with heat. Image courtesy of JAIC.
Care must be taken to not exceed temperatures higher than 100 C for this procedure. This is because tissue ablation, vaporization and carbonization can occur. Coagulation is one of the key processes in tissue welding, and lasers are used to induce this in tissues.
Tissue Welding Using Lasers
The ultimate goal of tissue welding is to obtain minimal scar formation for the surrounding tissue, and good tensile strength. High tensile strength is needed so that the welded tissues do not break apart. Usually a soldering biomaterial is used for this purpose. The image below shows an example of vascular tissue welding with albumen as the soldering biomaterial.
Albumen used as a soldering material while performing anastomosis.
After the laser heats the tissues in the junction to bring about denaturation along with the soldering biomaterial, the substructure is allowed to cool down. During this step, renaturation through covalent and electrostatic bond formation among the tissues takes place to hold the whole junction. While advances in laser technology can improve the control of heat that is delivered, important advances in tissue welding involves ingenious choices for the soldering material to give high tensile strength.
Lasers for Tissue Welding
The function of lasers in welding is to bring about efficient delivery of heat to the tissues in the junction. The main molecules that absorb heat are water, hemoglobin, and melanin. Water has strong absorption in the NIR region. This makes the use of solid-state and CO2 lasers ideal for water based heating. In contrast, if one is working with welding in blood vessels, one can target heating though hemoglobin. Since hemoglobin absorbs strongly in the visible region, Argon lasers, some diode lasers, and frequency doubled Nd:YAG lasers can be used for this purpose.
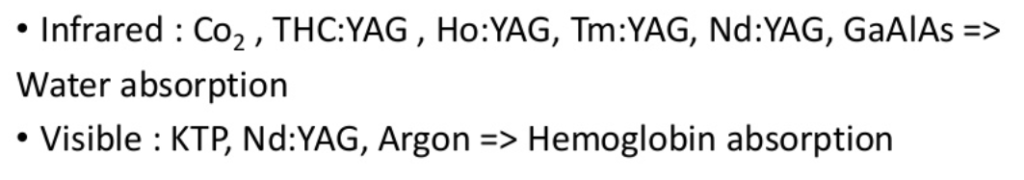
Different lasers for welding based on wavelength. Courtesy Slideshare.
Depending on the body tissue being soldered, there are various temperature limitations. One should also note that the optimal temperature for collagen bonding is within 60-80 C. Diode lasers used for vascular welding operate at around 80 C. Argon lasers used for arterial vein anastomosis heat the tissue to approximately 70 C.
Soldering Biomaterials
The common soldering material that has been used in such procedures is albumen. This is because, renaturation causes the soldering protein in albumen to be tangled up with the collagen molecules and increase adhesion. To further increase the strength of adhesion, researchers have been experimenting with many different types for particles such as gold nanoparticles.
Gold nanoparticles can be designed to strongly absorb light in the NIR region, such as near 800 nm. Diode lasers tuned to this wavelength can be used deliver the thermal energy necessary for denaturation. Gold nanoparticles are able to absorb more strongly and give higher absorption cross-sections than albumen, with a more uniform spread of energy causing the weld to be stronger when it is renatured.
Setup for Welding and Imaging
Below is a simple schematic diagram of a typical welding setup that uses diode lasers. In the setup, two different wavelength are used for the process. One wavelength is used to deliver thermal energy, and the other is used for imaging purposes.
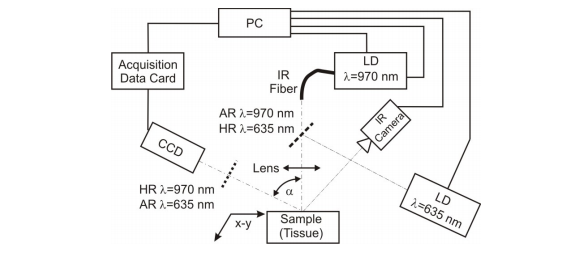
Use of laser diode in tissue welding. 635 nm laser diode along with the IR camera is used for imaging. Courtesy IEEE.
Laser light is delivered to the sample using an infrared optical fiber. The rate of heat delivered can be monitored using an IR camera.
Uses of Tissue Welding
While laser welding in tissues such as blood vessels and skin have been demonstrated, expanding the application to different biological tissues is necessary. For example, laser welding in urology requires the seal to be water-tight, so that water exposed non-lithogenic closures remain intact during continuous liquid flow. It is important to note here, that tight closures in urology lack the benefit of vascular tissues, where blood flow can clot microscopic leaks.
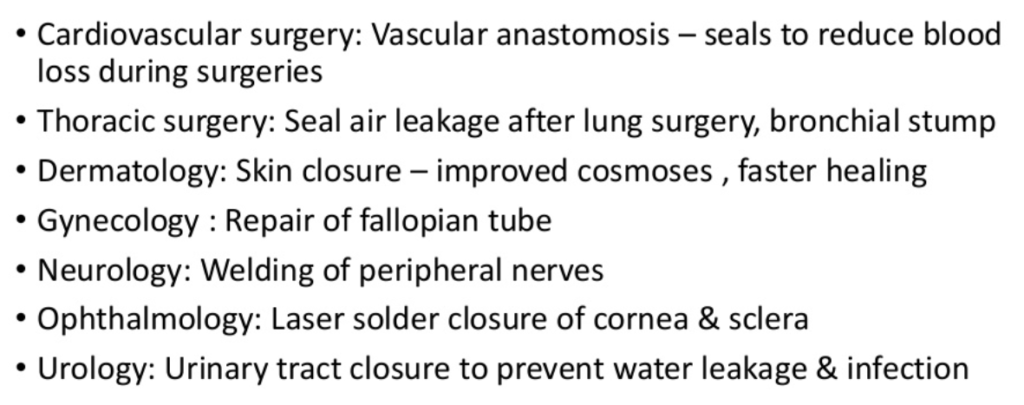
Different medical fields that benefit from laser tissue welding. Courtesy Slideshare.
In this article, we discussed the uses of Argon, diode and solid-state lasers in the visible and NIR region for tissue welding applications. Checkout FindLight’s collection of diode lasers, solid state lasers, and fiber optic accessories to use them in your designs.

Can blood used as a soldering material?
That’s a good question, since blood is a known coagulant