Cardiovascular diseases are among the top causes of death and morbidity in developed nations. In particular, diseases of the coronary arteries are most prevalent. Lasers are well suited to diagnose and treat these diseases, because of their standard implementation through fiber-optics that can be directly placed in the diseased vessels. One such application is the use of lasers to create transmyocardial incisions to increase oxygen supply to the heart muscles.
Lasers can be used to create transmyocardial incisions. This has many benefits as the procedure is minimally invasive. Plus the vast variety of lasers available has helped researchers experiment and come up with the ideal choice for creating incisions. It turns out, CO2 and Ho:YAG are currently the two most used lasers for transmyocardial procedures.
This article discusses the limitations of other surgical procedures to treat contraction of coronary arteries; the method and advantages of Transmyocardial Laser Revascularization (TMR); the use to Laser Doppler Flowmetry (LDF) to aid monitoring the increase in vascular flow; and the common lasers used for these purposes.
Heart diseases resulting from plaque formation in the coronary artery is shown in the image below. This can be treated with angioplasty. However, patients who have angina suffer from severe narrowing of the coronary arteries. As a result the heart does not receive as much oxygen-rich blood resulting in reduced blood flow called ischemia. This condition cannot be improved or corrected by angioplasty or a bypass. For some time, a heart transplant was the only option available for such patients.

Restricted flow in a coronary artery causing decreased oxygen supply. Courtesy MedicineNet.
How does TMR work?
Transmyocardial revascularization (TMR) remedies this by using laser to create vascular tissues to supply blood to the the outer walls of the heart. The method was called “snake heart procedure” for sometime, in analogy with reptilian hearts that supply blood to the heart muscle through channels that extend from heart chambers.
In a transmyocardial procedure, high energy pulsed laser beams are used to create 20 to 40 incisions from the outer wall to the left ventricle. Each incision is about a millimeter in diameter. The incisions allow blood to carry oxygen to the outer walls of the heart. The holes in the heart are clotted to be sealed shut and heal within days. Over the months, these incisions promote angiogenesis, which is the formation of new vascular tissue on the outer walls of the heart.
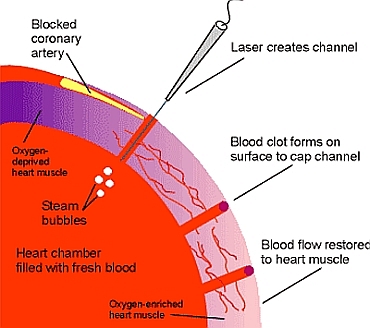
Cross section of Tranmyocardial incisions.Courtesy UWHealth.
Transmyocardial procedure has several advantages compared to other procedures. Most importantly, the heart is not stopped as in a bypass surgery, and the procedure is a lot less invasive compared with an open heart surgery. The procedure does however require an incision between the patients ribs to reach to the heart as shown in the image below.
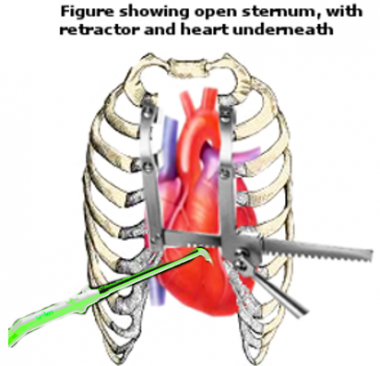
Chest incisions for laser energy livery in TMR. Courtesy Medscape.
Not surprisingly, TMR has also a faster recovery time compared to a bypass surgery. Medicinal researchers are currently exploring the use of so-called percutaneous TMR (PTMR) to prevent the need of a chest incision to reach the heart. In PTMR, the laser energy is delivered through a catheter inserted through an artery to reach the heart.
Laser Doppler Flowmetry for Transmyocardial Surgery
TMR procedure requires monitoring the blood flow in the newly formed vascular tissue and reading flow levels right below the clotted region. Laser doppler flowmetry (LDF) is the primary technique for this purpose. To measure the flow rate, doctors use emitting and receiving fibers to register the reflected from hemoglobin light. The received Doppler shifted wavelength provides information about the velocity of the blood cells. The image below shows a simple setup using LDF during such a heart surgery.
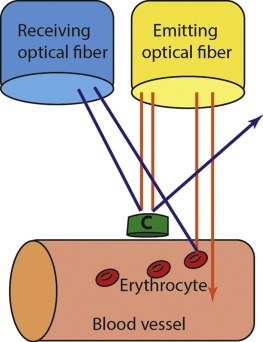
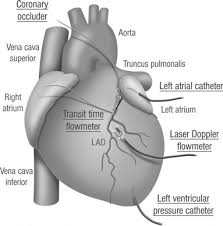
Top: Idea behind Doppler Flowmetry. Bottom: Use in TMR. Courtesy ResearchGate.
Lasers in Transmyocardial Surgery
The most effective lasers for TMR are CO2 and Ho:YAG. Other lasers such as Nd:YAG, Eb:YAG have been explored experimentally, but none have been pursed on a significant scale for clinical applications. At the moment, only CO2 and Ho:YAG are clinically approved for transmyocardial incisions.
CO2 operates at a wavelength of 10.6 um, and Ho:YAG at 2.12 um. The primary mechanism of tissue ablation for both of these lasers is the absorption of light by the water contained in the heart tissue. Since water absorbs strongly at these wavelengths, the transfer of energy is very efficient. Care must be taken while using the Ho:YAG laser in the pulsed mode. If significant time is not present between two pulses, accumulated heat can cause tissue to explode under pressure. The operation parameters for Ho:YAG is 6-8 W/pulse. The CO2 laser for TMR operates at a slightly higher pulse energy.
Post-Surgery Effects
Over the weeks of the surgery, the formed incisions promote angiogenesis. This is shown in the image below.
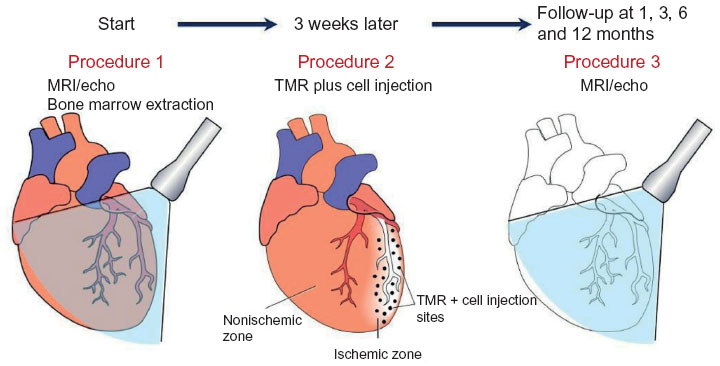
Stages for post-surgery effects. Courtesy Dovepress.
Most of the laser drilled channels are closed soon after the surgery. However, the short-lived flow of the blood through the channels continues to stimulate oxygen supply to the heart wall. Even though the theoretical details of why new blood vessels appear in TMR are not clear, its practical efficacy has been demonstrated. Since its FDA approval in 1998, it has been the only procedure for treating patients with severe coronary problems, with only patients with unstable angia or reduced left ventricular function not benefiting from this procedure. For more on TMR in medicine, check out the NCBI article.
Did you know, FindLight is a worldwide photonics marketplace with many premier suppliers of solid state lasers, CO2 lasers, and fiber optics accessories for controlling delivery of the laser output.
